Blood typing and transfusion worksheet – Embark on an exploration of blood typing and transfusion with our comprehensive worksheet, designed to unravel the intricacies of this critical medical procedure. This guide will equip you with a thorough understanding of blood typing principles, compatibility factors, and transfusion protocols, empowering you to navigate the complexities of blood transfusions with confidence.
Delve into the fundamentals of blood typing, unraveling the significance of blood groups, antigens, and antibodies. Discover the intricacies of blood compatibility, exploring the ABO and Rh systems and their role in determining compatibility. Gain insights into the potential consequences of transfusing incompatible blood, equipping yourself with the knowledge to mitigate risks.
Blood Typing Basics

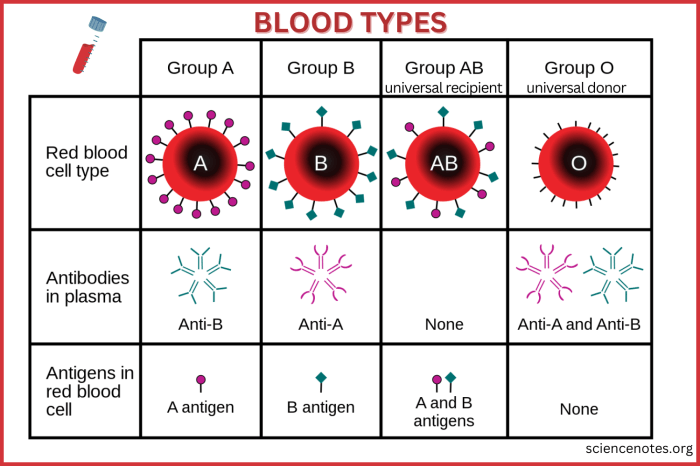
Blood typing is the process of determining the type of antigens present on the surface of red blood cells. Antigens are proteins that trigger an immune response when they are recognized as foreign by the body. The most important blood group systems are the ABO system and the Rh system.
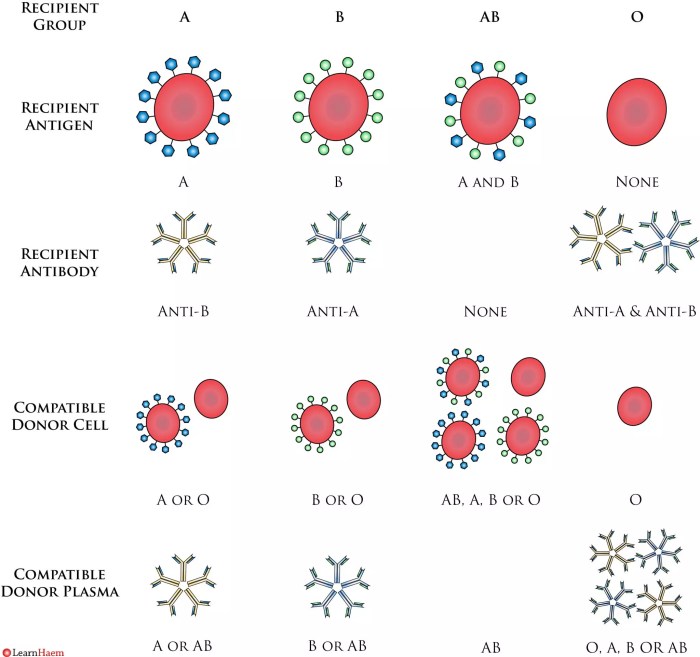
The ABO system has four main blood groups: A, B, AB, and O. People with type A blood have A antigens on their red blood cells, people with type B blood have B antigens, people with type AB blood have both A and B antigens, and people with type O blood have neither A nor B antigens.
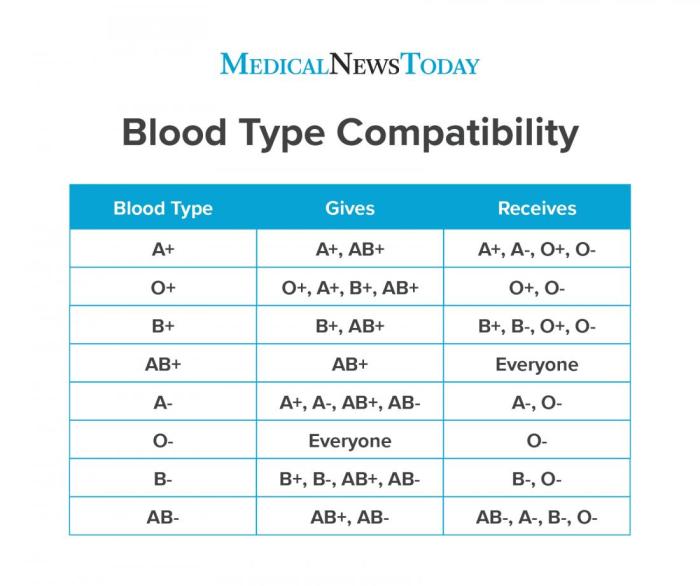
The Rh system is another important blood group system. People who have the Rh antigen on their red blood cells are Rh-positive, while those who do not have the Rh antigen are Rh-negative.
Compatibility and Transfusion Reactions, Blood typing and transfusion worksheet
Blood transfusions are only safe when the donor and recipient have compatible blood types. If a person receives a transfusion of incompatible blood, their immune system will attack the transfused red blood cells, causing a transfusion reaction.
The most common type of transfusion reaction is an ABO incompatibility reaction. This occurs when a person receives a transfusion of blood that contains antigens that are not present on their own red blood cells. For example, a person with type A blood cannot receive a transfusion of type B blood because their immune system will attack the B antigens on the transfused red blood cells.
Rh incompatibility reactions are less common than ABO incompatibility reactions. They occur when a person with Rh-negative blood receives a transfusion of Rh-positive blood. The recipient’s immune system will attack the Rh antigens on the transfused red blood cells.
Blood Typing Procedures
Blood typing is a simple procedure that can be performed in a laboratory. The first step is to collect a blood sample from the patient. The blood sample is then mixed with antibodies that are specific for the A and B antigens.
If the patient’s blood contains A antigens, the antibodies will cause the red blood cells to clump together, or agglutinate. If the patient’s blood contains B antigens, the antibodies will cause the red blood cells to agglutinate. If the patient’s blood does not contain A or B antigens, the antibodies will not cause the red blood cells to agglutinate.
The Rh factor can also be determined by mixing the patient’s blood with antibodies that are specific for the Rh antigen. If the patient’s blood contains the Rh antigen, the antibodies will cause the red blood cells to agglutinate.
Transfusion Protocols and Guidelines
There are strict protocols and guidelines in place to ensure the safety of blood transfusions. These protocols include:
- Patient identification:The patient’s identity must be verified before a blood transfusion can be given.
- Blood typing:The patient’s blood must be typed to determine their blood group and Rh factor.
- Cross-matching:The patient’s blood is mixed with the donor’s blood to ensure that the two blood types are compatible.
- Administration:The blood transfusion is administered slowly and carefully.
Special Considerations
There are some special considerations that must be taken into account when transfusing blood to certain patient populations, such as newborns, pregnant women, and individuals with rare blood types.
Newborns have a different blood type than adults. Their blood is typically type O and Rh-negative. This means that they can receive blood transfusions from any donor who is type O and Rh-negative. However, newborns cannot receive blood transfusions from donors who are type A, B, or AB because their immune systems will attack the transfused red blood cells.
Pregnant women can develop antibodies to the Rh antigen if they are Rh-negative and carrying an Rh-positive fetus. These antibodies can cross the placenta and attack the fetus’s red blood cells, causing a condition called erythroblastosis fetalis. To prevent erythroblastosis fetalis, Rh-negative pregnant women are given a medication called RhoGAM.
Individuals with rare blood types may have difficulty finding compatible blood for transfusions. In some cases, they may need to receive blood from a donor who has the same rare blood type.
FAQ Summary: Blood Typing And Transfusion Worksheet
What is the significance of blood typing in transfusions?
Blood typing determines compatibility between donor and recipient blood, preventing potentially life-threatening transfusion reactions.
How does the ABO system determine blood compatibility?
The ABO system classifies blood into four groups (A, B, AB, O) based on the presence or absence of A and B antigens on red blood cells.
What are the signs and symptoms of a transfusion reaction?
Transfusion reactions can range from mild (fever, chills) to severe (hemolytic reactions, anaphylaxis). Prompt recognition and treatment are crucial.